My Story
Author – Amy Laura (USA)
How eating low FODMAP for 3 days began to calm 30 years of chronic digestive distress and pain …
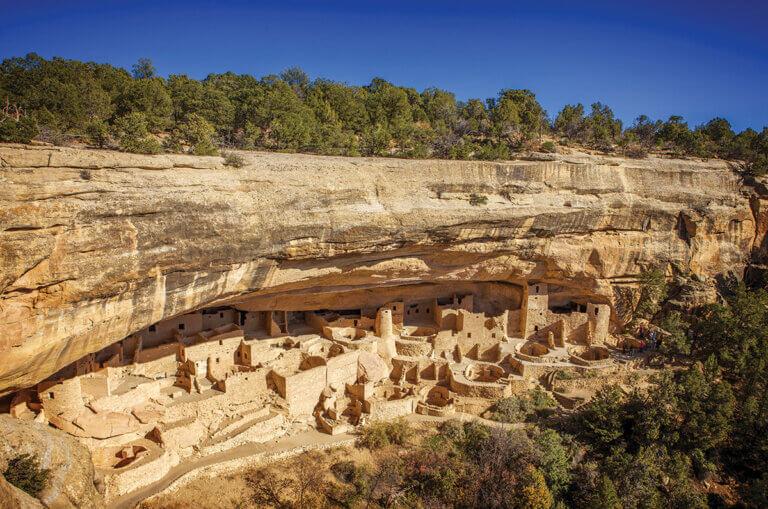
Hi there! I’m Amy – a FODMAPer, cookbook author, photographer, national parks and historic district enthusiast, gluten-free bakery stalker, and avid home cook. I live in the Four Corners region of the American Southwest on a ranch with my darling husband Jim, a group of big-hearted people, two little dachshunds, and twenty-six dogs who belong to the ranch and think of me as Auntie Cookie. One of my greatest joys is to fill my pockets with doggie treats and walk out to the play yard.



Tap here for My Story short version on the Monash FODMAP Blog.
If you are new to the Low FODMAP Diet, Tap here for our brief explanation page.
I believe that when you have a chronic illness and find something that offers relief – in my case life-changing relief – this information should be shared with others who are seeking answers.
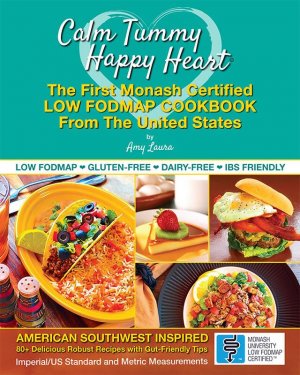
I wrote Calm Tummy Happy Heart cookbook because for most of my life I suffered from unpredictable, misdiagnosed and oftentimes severely painful digestive symptoms due to Irritable Bowel Syndrome (IBS-D). Calm Tummy Happy Heart is the First Low FODMAP Cookbook from the United States with 80+ recipes assessed and certified under the Monash University Low FODMAP Certification Program for recipes.
The Monash University Department of Gastroenterology of Melbourne, Australia researched, developed and invented the Low FODMAP Diet to manage IBS symptoms. I think of them as the Mothership of FODMAP research.
It is my wish to offer help by sharing recipes, symptom relief tips, and my journey in finding answers, because it was through reading about the personal experiences of others that had me nodding my head “I know how that feels, yes, that’s me.” This was the manner in which I discovered the Low FODMAP Diet that has given me the gift of a calm tummy, empowerment in finally knowing how to manage my condition, and comfort that lifts my heart with happiness and hope.
Tap here to sign up for my FODify It! newsletter and receive 3 free certified recipes from the cookbook, plus an extra bonus sneak peek.
There is no single known cause or cure for IBS. The good news is that it is not contagious and we can find ways to alleviate the symptoms. In the past few years, the Low FODMAP Diet has found it’s way onto the radar of U.S. health publications, general physicians, gastroenterologists and cookbooks. There are now U.S.-based low FODMAP meal delivery services and food brands specifically tailored to the diet. This gives me comfort that awareness is building, because 1 in 7 people are affected by IBS and 75% find relief through this food regimen.
The details of my search for answers is lengthy due to thirty years of trial and error, and I’ve intentionally included as much as I can recall because if you or someone you know suffers from IBS and relates to even a portion of my story, it is my hope that these examples will lead to ending the discomfort and confusion they are going through by trying the Low FODMAP Diet. And to not feel so alone in this as I did.
HOW DID I GET IBS?
When I was in school, I shared lunch with a classmate who went home later that day and collapsed from meningitis. She was taken to the hospital and placed in the Intensive Care Unit. Thankfully, she completely recovered. As a precaution, I was quarantined and given heavy doses of medications. I never contracted meningitis, but shortly after this incident my IBS symptoms began with sharp abdominal cramping, random diarrhea upsets, bloating, fatigue, brain fog, gas, feeling overheated and flushed, and eventual fluky bouts of anxiety.
I would later learn that a few members of my family have sensitive digestion, indicating that I was genetically predisposed, and the heavy meds triggered my IBS. I also went through a series of dental procedures that required prolonged use of antibiotics – another IBS instigator.
THE SEARCH FOR ANSWERS
Early on, I consulted my doctor and gastroenterologist with concerns that I felt like I was being food poisoned or might be allergic to something. The abdominal cramping, pain, and random stomach flare-ups were happening several times a week and I was taking over-the-counter drugstore anti-acids to get by and make it to school and work.
My physicians were caring, concerned and baffled about what was happening with my body. Very little was known about IBS when my symptoms began in the 1980s. It was called spastic colon then, and it would be decades until IBS or FODMAPs were on mine or my doctor’s radar.
Before delving further into my story, I want to mention that countless chapters of my life have been positively joyful. Sure, I’ve missed out on family celebrations, had to cancel countless plans and missed special events because of my condition. But many times I’ve felt like my life was and is a great book I’ve picked up and I cannot wait to turn the next page. I’ve also been known to laugh in my sleep, so I want to be sure to convey that my life hasn’t been an entire existence of cheerless bummed-out tummy drama.
Still, it was a long journey that affected the quality of my life on a daily basis, and changed the course of my plans and career.
GETTING TESTED
If you are suffering from the symptoms of IBS it is critical that you go through testing with a gastroenterologist to rule out other conditions that may be the cause, or life threatening. It is important to note that home tests are not reliable or supported by reputable RDs or MDs at the time of this writing.
My search began with allergy panels. All tests came back negative including wheat and dairy. Years later I would learn that the body can have sensitivities to certain foods that do not show up on allergy panels.
Next came a gastrointestinal series of x-rays, colonoscopies and more tests. All came back clear along with the first diagnosis that I needed to meditate and handle my stress better because it was “all in my head.” After all, my tests were negative so what else could it be?
I feel it’s important to lay it on the line that I never believed it was all in my head. Anxiety can be an IBS trigger, but I’d been on vacations that were entirely designed around relaxation. While on these rejuvenation trips I had flare-ups and abdominal pain. My gut instinct knew that there was something more to it.
Can meditation, good counseling for anxiety, and exercise help to soothe digestive upsets? Absolutely. Anxiety and stress play a part in IBS symptom flare-ups because the gut and brain are always talking to each other. But for me, one who is highly sensitive to FODMAPs, I was still in digestive discomfort because I had no idea how to FODify It! – modify the FODMAPs in my diet.
FOOD ELIMINATIONS
I began eliminating specific foods from my diet one by one and kept a food journal to track the progress. Still suspicious of dairy, sugar and wheat (bye bye flour tortillas!) I individually eliminated them. No relief came from giving up dairy or sugar, but my symptoms did slightly improve by going gluten-free. I later learned that the fructans in wheat make it one of the greatest FODMAP offenders, so it made sense that I would feel a bit of relief. But giving up wheat and going gluten-free alone was not enough for my sensitivities, and the upsets soon returned.
BLAND FOODS
My next effort was to try bland foods such as: rice, potatoes, oatmeal, flour and corn tortillas, vegetable soups, saltine crackers, puréed vegetables (like homemade baby foods), minced chicken and clear sodas. Again, no relief. What I didn’t know was that along with these foods I was mixing in onion, garlic, dairy, stone fruits, high fructose corn syrup (from the sodas), and other ingredients containing high amounts of FODMAPs.
I also drank lots of chamomile tea that is high FODMAP. Low FODMAP swaps for this are peppermint and ginger tea, to name a few.
FASTING
I must have been quite desperate to try fasting and juicing because I’d known for years that if my stomach became empty it would growl. Loudly. Just imagine the sounds of handing a metal pie tin full of marbles to a raccoon to play with. I’m only slightly exaggerating here. Then came GI upsets, so fasting was out.
GARLIC
In the 1990s, health magazines began printing articles on foods that were purportedly antioxidants and reduced hypertension and cholesterol. Garlic was high on the list, so I would frequent a garlic-themed restaurant that was known for 40-clove garlic infused chicken, garlic ice cream, and garlic everything. My stomach would become so bloated it looked like I’d eaten 25 pounds of tofu. “Was it the clams? Did I eat too much bread? It can’t be the garlic. Garlic is healthy.”
I began wearing clothes that were two to four sizes larger in order to hide my tummy. And to this day, from years of being bloated with abdominal cramping, I still wear huge shirts and dresses because I don’t like to feel my clothes touching my body.

It turns out that garlic (and onion) contain fructans, and if you are sensitive to this FODMAP you need an alternative strategy. The LoFO swap is that we can properly infuse oil with garlic and onion to get around the fructans (which are not oil soluble) and still enjoy their pungent, aromatic flavors.
For example, if you were to make a Pork Posole Stew, drop in a few pieces of garlic and onion, let it simmer and remove the pieces before serving, the fructans will have leached into the stew. They’re still in there and this may very well trigger your symptoms. However, were you to heat canola or olive oil (the two I most often cook with) in a pan, add garlic and onion pieces, let them slowly infuse into the oil, then remove all of the pieces, you are left with a flavorful infused oil to cook with. Sans fructans.
A few more LoFO swaps for the white bulb of onions are: green parts of scallions, leek leaves and chive stems. Green parts only.
More good news is that in the Reintroduction Phase of the diet, many people find that garlic and onion are no longer a digestive trigger.
PILLS INCIDENT
I want to preface this next experience by noting that there are medications that help people with the symptoms of IBS. The following incident took place twenty years ago and since then there have been improvements in understanding GI conditions and drug research that offer relief. Unfortunately, I had a dicey experience with a medication.
A top gastroenterologist in his field handed me a prescription for a medication that was “helping thousands of women” with my symptoms. This was a highly recommended Los Angeles doc so I immediately took the pills. The next day, I left for a travel assignment and began to feel nausea, loss of appetite, abdominal cramping, headaches and brain fog. I stopped taking the pills and once home, went for a follow-up exam. The doc looked at my chart and said “You’re not still taking these pills, are you? They’ve been causing intestinal bleeding.” The lesson I learned that day was: no matter who writes the prescription, research the blazes out of it before you take it, and even if it is a supported drug, listen to your body. If it doesn’t work for you, advocate for yourself with your GI.
Still, I held onto the belief that you are never defeated until you give up, and continued my search to be properly diagnosed with a proven treatment plan.

VEGAN + VEGETARIAN
Later came parasite tests, more x-rays, blood tests and consultations with a few highly recommended gastroenterologists.
I was vegan for almost two years, then vegetarian for several years and my symptoms during both food phases, to my amazement, worsened. My foods contained high FODMAPs found in cauliflower steaks, cashew butter, wheat flour tortillas, refried and various beans, salsas with garlic and onion, and certain vegan soy products that aggravated my digestion.
Don’t be worried if you are vegan or veggo. It is possible to FODify your foods and you can find tips and notes at monashfodmap.com.
HOLISTIC TREATMENTS
Next came a costly health food delivery program, but no tummy relief. Then meeting with a holistic practice that everyone was writing and raving about. They created calming tinctures and tea blends, we sat on big poofy pillows and meditated together, and I quickly fell in love with this quiet place of lowly lit rooms with incense hovering around us. I spent a small fortune, and when nothing worked we were all puzzled. But at least I had learned new tools for living and communicating through their mindfulness teachings.
PSYCHOTHERAPY
I’m a strong believer in psychotherapy as an objective touchstone during difficult times and life changes, and have sought the help of therapists over the years to help me with not feeling present in my life. I didn’t trust my body and really, why should I have? The next random upset with pain could happen at any time and that worry was always in the back of my mind, far too often distracting me from fully enjoying my life.
During these sessions, the focus was on childhood experiences and current life situations. When I brought up my digestive issues they were not examined as a part of my treatment. I began to feel the “it’s all in your mind” vibe again. This is why I am elated that today, because of the Monash team and publications of GI related articles that raise awareness for a more open attitude in discussing GI conditions, I have a therapist who specializes in chronic illnesses and anxiety, a general physician who is familiar with the Low FODMAP Diet, and my gastroenterologist is also on the plan. Things in the therapy and GI world have come a long way in 30+ years.
SOCIAL LIFE AND WORK
In order to have a social life, make it to work and have as normal a lifestyle as possible, I managed by continuing the over-the-counter antacids and other drugstore tablets that semi-calmed my symptoms but merely masked the problem. Please know that I am not encouraging self-medicating like this. This was something I did just to get by, and not one gastroenterologist I’ve consulted with has recommended prolonged use of these drugstore digestive aides.
In Southern California, I was living the life I’d trained for and always wanted – to work in my field of photography, travel to places I’d might never have had the opportunity to explore, and meet new, interesting people every day. It was fast-paced, hurrying through breakfast, long hours with little sleep, catching planes, setting up location situations on travel days, eating dinner at 11pm, and for years I absolutely loved it.
The downside was that over time my symptoms became worse. Lack of sleep, not properly chewing my food, eating high FODMAP foods, and the pressure of shooting negative film that needed processing at a lab, editing, packaging and then driving it to the airport to overnight ship to the client were all adding up.
I remember a photo assistant I’d worked with who was so sleep deprived after a very long location shoot, he shipped his personal mail to the client and dropped the shot film package in a mailbox. I recall many late night drives home with the unease of getting into gridlocked traffic with no access to a bathroom, and then driving back to the location in the morning where no one could leave the set because our time was limited with the talent. That was panicky for me and my unpredictable tummy. Many people I’ve spoken with who suffer from IBS feel the workplace pressure of limited breaks and long commutes.

Conversations about my condition were reserved for family, a few close friends and my doctors. If word got around that I had a chronic illness, or if I had to cancel last minute on an assignment, I would be replaced. That was and is the nature of freelance employment in the overnight photo deadline machine where “the show must go on” also applies.
People began to comment that I sounded fine but my eyes looked very tired. My response was that I was going through a phase of insomnia. I’ve recently learned from a friend that another good excuse during social events is “I have lower back issues and need to excuse myself and lie down flat for a bit.” Backaches are easier and less embarrassing to explain than IBS problems.
Eventually, due to increased symptom flare-ups and fatigue, I began arranging to work from home and gradually, reluctantly turned down travel assignments. This change brought on depression as I gave up the wanderlust lifestyle I’d always planned for, and I generally ventured no more than 10 minutes from my house. That’s how bad and frequent the upsets had become. I didn’t trust my body, had no answers to take action and heal, and it was finally all too much to handle.
Many people with chronic GI issues have revealed that they would give up 2 or 3 years of their lives to live free of their condition right now and for the remainder of their lives. At this point in my life, I related to this. Science tells us you cannot die from IBS, but the symptoms can sometimes feel that severe.
MY BIG MISTAKE
We all make mistakes and this one became an important life lesson. Around the 20ish year mark of my IBS onset, I was mentally and physically exhausted. Feeling hopeless, I rejected my mantra that we are never defeated until we give up and discontinued my GI appointments and search for answers.
During this time, huge strides were being made in gastrointestinal research, FODMAPs and the gut-brain axis relation to IBS. Had I stuck with my mantra, I would have found relief years earlier.
Then one night while I was getting ready to meet friends for dinner, I collapsed. I had doubled over with abdominal pain before but this one was different. I fell to the floor and could not get up or move out of the fetal position. The sharp pain kept coming in waves. I was sicker then I’d realized. After a bad flare-up it took some time to recover. I canceled the dinner, made an appointment with my doctor, and went online to look up my symptoms again. The same strange acronym kept popping up – FODMAP. A food program for IBS relief? Food as medicine? I found a few online lists of low FODMAP foods, woke up the next morning, drove to the market and stocked my kitchen with a week’s supply of ingredients to test on myself.
IT WORKED
Within three days – and I will never forget this – I was sitting in the living room with Jim. We were watching a movie and I suddenly realized that my body had been peaceful all day. I had eaten strictly LoFO foods, my stomach was calm, not at all bloated and I had no brain fog, discomfort or pain. After three decades I felt significant relief! I remember smiling that I might be able to trust my body again and leaned back as if I was melting with happiness right into the sofa. “But will this last?” I also wondered.
Two months later, I was on a natural high having gained a huge boost of energy and my digestion was so improved that I woke up each morning with a newfound sense of normalcy and understanding of how to manage my condition. I had also consulted with my GI, worked with a few dietitians and soon realized that I was getting my life back!

TODAY
Rather than dwelling on times of hopelessness and feelings that “Life isn’t fair,” and “Why did I have to go through all of this?” I channel these thoughts into being thankful for where I am now with my health, and how lucky I am to have the knowledge to calm my symptoms.
I have a chronic illness, found something that gives me relief, and I will do anything to maintain this feeling of freedom and bliss. I continue to follow the Monash 3-Phase plan, reintroduce foods into my diet, and find my balance of maintenance through foods and mindfulness.
I follow the Monash and FODMAP community online for updates on research and newly tested foods, to hear their stories, humor, triumphs and setbacks, and am eternally grateful to be a part of this supportive community.
If I have an occasional flare-up or if my sleep is off, my body will tell me that I need to eat strictly low FODMAP for a few days and rest. I’m far more mindful of that now. I still have bouts of anxiety and know the value of a support system in getting through difficult times. But even so, I’ve never felt so comfortable in my own skin, and the word grateful seems to come up in conversation almost every day.
I’m able to travel again without the uneasiness of a distracted mind. The five hour drive from Santa Fe to Mesa Verde National Park is a pleasure that I am able to enjoy and feel present in the moment.
COOKBOOK
When I first realized I had complex food sensitivities (and even beyond FODMAPs from skins of fruits and vegetables, and MSG) I was worried about what I’d have to give up. I mean, what about fajitas, spicy chocolate brownies, green chile burgers, gazpacho and other dishes containing high FODMAP ingredients? Not to mention, a life without green chiles would be like a sky without stars. My assumption was that low FODMAP meant bland foods with no flavor. Boy was I wrong.
I began flipping through my recipe box and converting my best efforts and dishes I was craving with appropriate LoFO food swaps. It took no time at all to realize that I did not have to give up the flavors and foods that are a big part of my regional cuisine. I could FODify It! by using the Monash FODMAP smartphone app to swap out certain foods in proper portions. And could cook with high FODMAP ingredients such as avocados and jalapeno peppers by measuring out their low FODMAP portion sizes per serving.
A few years after this epiphany, I had the makings of a cookbook with traditional, robust Southwest recipes that satisfied my cravings so that I never felt deprived of the foods I love. I needed to share this. Through working with the Monash FODMAP Team, this initial inspiration became a volume of recipes offering the home cook confidence in making Monash FODMAP Certified recipes for a calm tummy, and empowerment to lift your heart with happiness, hence the book’s title.

RELIEF FOR YOU
I want you to know that if you are relating to my story, I am sorry. Because I know the pain and disruption this has on your life. I wish I were there to give you a big hug right now. This is why I feel it is my calling to share my story, create cookbooks and offer helpful resources through FODify It! – my online resource for low FODMAP symptom relief, lifestyle tips, and recipes that are inspired by the American Southwest.
Once we have answers, we know how to make decisions to improve our health. That’s what I wanted and daydreamed about for so long – a scientifically proven method to manage my symptoms without all of the guessing.
I hope you will try the Low FODMAP Diet and find relief. I hope my recipes and resources will help you. I can tell you from experience that working with a physician to first rule out other possible causes of your symptoms, and a Monash Certified dietitian will make the journey easier and you will be far more informed. Stick with your journal to track which foods are triggers or okay for you, take the online Monash FODMAP Patient Course (you will need the app for this), and if for some reason your body does not adapt to the diet, do not give up your search for answers and a proper diagnosis.
If you are already LoFO, I hope you enjoy my recipes and that they help you to never feel deprived of the robust richness of American Southwest foods.
Wishing you a calm tummy and happy heart.
Amy
Buy The Cookbook – Barnes & Noble
3 Free Certified Recipes from the Cookbook with FODify It! Newsletter Sign-Up
Low FODMAP Southwestern Food Swaps
Disclaimer: the information included in My Story, FODify It! website and Calm Tummy Happy Heart cookbook are intended for educational and informational purposes only. Content provided in My Story and the cookbook are not a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or another qualified healthcare provider before altering your diet or modifying an existing treatment plan.